Advancing Medical Training by Choosing the Right Simulation Models
Written by Donya Mand, M.D.
August 2024
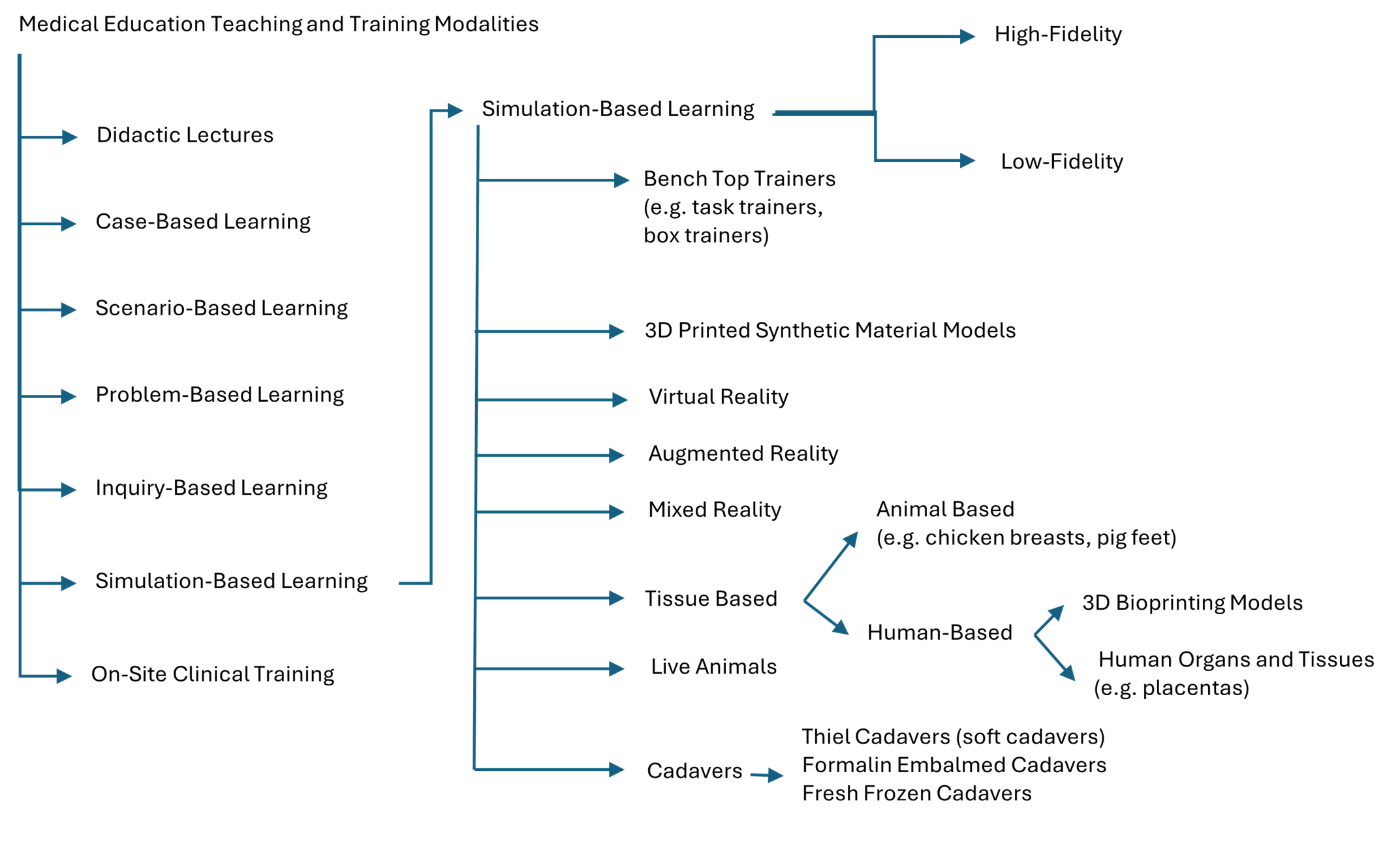
Medical education for physicians encompasses various skill levels and sets, including training for undergraduate medical students, physician residents, and graduate fellows and continuing education courses for practicing physicians. The modalities used for medical training are broad, with different levels of applicability depending on the trainee’s current education level and professional specialty. Medical education and training methods include didactic lectures; case-based, scenario-based, problem-based, and inquiry-based active-learning activities; simulation-based training; and on-site clinical training.
Trainees’ professors and peers present didactic lectures, which are content-centered and focus on informing them about certain topics while they passively listen. Active-learning activities encourage trainees to work independently or collaboratively to think through different cases, scenarios, problems, or questions. In on-site clinical training, students and trainees with either indirect or direct oversight observe, learn, and practice skills in an environment involving actual patients.
Within simulation-based medical education and training, there are many subtypes based on where the simulation model is used, which materials make up the model, and which technologies are employed: bench-top models, 3-D printed models, virtual reality, augmented reality, mixed reality, animal tissue–based simulators, live-animal simulation models, human tissue–based simulators, and human cadavers. Simulation models are further classified as low- or high-fidelity models based on how similar the simulation is to the real-life experience of practicing that skill. What classifies as low or high fidelity is subjective and changes as technologies evolve. Low-fidelity simulation models, which are usually benchtop models and animal-part models, are the least realistic. High-fidelity simulation models, such as high-quality virtual technologies, human cadavers, and, at present, certain live-animal models, are the most realistic. The following classes of simulation models are the most popular:
- Benchtop models are used outside a clinical environment, often sit atop a laboratory bench, and focus on teaching basic and specific skills. These models are often called task trainers or box trainers.
- 3-D printed models are made of synthetic materials or bioprinted with human cells.
- Virtual immersive technologies are either virtual reality (VR), augmented reality (AR), or mixed reality, which combines VR and AR.
- Animal tissue–based simulators often use animal parts, such as chicken breasts or pig feet, purchased from a grocery store.
- Live-animal simulation models use various animal species, including dogs, cats, piglets, rats, and mice, to practice procedural and surgical skills while the animal is under anesthesia. The animals are killed at the end of the training session.
- Human tissue–based simulators can be bioprinted or include a specific human organ (e.g., a placenta).
- Human cadavers are often considered the gold standard for practicing surgical and procedural skills, and their preservation method is based on whether the objective is to maintain them in a “lifelike” state or to preserve them for long-term use.
Simulation models that were considered to be high-fidelity 20 years ago may fall out of favor as more advanced models supersede them. For example, laparoscopic training often relied on live animals as high-fidelity models, but now VR laparoscopic simulators are also considered high-fidelity, often proving just as effective as live animals in teaching laparoscopic surgery.1,2
The transition to non-animal simulation methods is already in process, with many institutions ending their reliance on animal-based models for surgical and procedural training. Medical educators can help continue to make this shift by focusing on more human-relevant simulation models that are both ethical and effective in the following ways.
- Replacing live animal–based models with VR and AR models: Although cost is often cited as a barrier, the financial burden of VR and AR models is decreasing yearly. Unlike live-animal models, these tools can be reused for multiple training sessions over many years without needing to hire specialized staff to maintain and transport animals.
- Replacing animal tissue with 3-D printed synthetic materials or bioprinted models from human cells: These models allow trainees to work with surgical and procedural tools that are more anatomically and tactilely similar to real patients. 3-D printed synthetic materials can mimic human anatomy and be designed to show a variety of pathologies that can’t be replicated in animal tissue, thereby providing greater opportunities for trainees to practice on more challenging cases. Bioprinted models that use human cells can also provide a realistic stand-in for human tissue.
- Collaborating with trainees in multiple specializations to use every component of a human cadaver fully: Whole human cadavers are often used for specialized training, but not all parts of a cadaver are useful for every specialization. One cadaver can be used for training in general surgery on the abdomen, neurosurgery on the brain, ophthalmology on the eyes, orthopedic surgery on the extremities, and plastic surgery on the hands and by creating skin flaps.
Selecting the right simulation models is crucial for comprehensive and effective medical training at all levels, and as technology evolves, so must the training tools. The shift from traditional animal-based simulations to advanced, human-relevant models like VR tools and 3D-printed materials marks a significant advancement, offering better anatomical accuracy and cost-effectiveness. Transitioning away from animal tissue–based models also helps prevent the potential spread of zoonotic diseases. A diverse array of simulation models is essential to equip trainees with the skills necessary for procedures on humans. Training curricula should be regularly updated to ensure the use of the most effective and ethical models, enhancing medical education and improving patient care.
1Bian Z, Zhang Y, Ye G, Guo F, Mu Y, Fan Y, Zhou X, Zheng Q, Konge L, Wang Z. Laparoscopic training on virtual-reality simulators or live pigs—a randomized controlled trial. Ann Med Surg (Lond). 2023 Jun 5;85(7):3491-3496. doi:10.1097/MS9.0000000000000798. PMID: 37427191; PMCID: PMC10328584
2Samia H, Khan S, Lawrence J, Delaney CP. Simulation and its role in training. Clin Colon Rectal Surg. 2013 Mar;26(1):47-55. doi:10.1055/s-0033-1333661. PMID: 24436648; PMCID: PMC3699140.

